Repeating a skin test cannot possibly assess the efficacy of allergy treatments, and will likely disappoint your patient.
By: MRS Allergy Medical Director Dean C. Mitchell, MD, Board Certified Immunologist and author of Allergy & Asthma Solution
Allergy prick skin testing is considered the gold-standard for diagnosing immediate allergy to environmental substances and foods.
MRS Allergy is carefully training doctors all over the United States how to perform prick skin testing properly. In the past, allergy skin testing was mainly done by allergists and ENTs, but this has changed in recent years. Today, pediatricians, family physicians, related specialties (ophthalmology and dermatology) and even urgent care physicians are using this testing to specifically diagnose their patient’s allergic symptoms, and treat them.
Desensitization: IgE Reactions Blocked by IgG Stimulation
IgE is associated with immediate allergic reactions that are associated with airborne allergens such as: dust mites, animal dander, pollen and molds. It also involved in sometimes dangerous reactions to foods such as peanuts and shellfish. Allergy prick skin testing measures the allergen’s effect on IgE on the patient’s skin cells. Being pricked with a tiny amount of a substance to which the patient is allergic will set off a histamine type IgE reaction within 15 minutes of application that can then be easily measured for the size of the induration (swelling–not the redness), which indicates the severity of the allergy.
Patients who show a positive reaction to an allergy skin test reflect an IgE reaction, and if their clinical history matches up are accordingly diagnosed with clinical allergy. In the past, then patients had a limited choice of taking daily antihistamines of various varieties or nasal corticosteroid sprays (e.g. Flonase) to achieve some relief, and/or receiving allergy injections to suppress their symptoms long term. Antihistamines and steroids don’t block the IgE response, and only relieve symptoms very temporarily, while injections entail weekly visits to the doctor’s office for months on end, each one lasting at least half an hour plus travel and wait time. Today, through MRS, patients have a third choice: sublingual allergy drops at home to reduce and suppress their allergies for the long term.
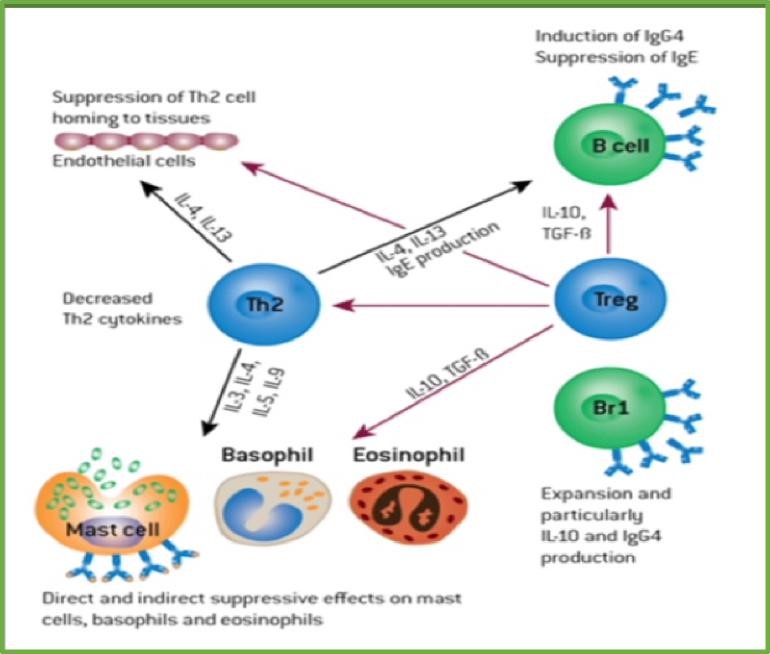
How? Allergy immunotherapy is also referred to as desensitization–meaning the patients are given the actual allergen(s) they are allergic to initially in very small doses that over a period of months increase in allergen concentration. Dosage increases until the patient reaches a maintenance dose, which taken for a sufficiently long time trains the patient’s immune system not to have an IgE reaction and thus suppressing the symptoms for years after the therapy concludes.
The immunological mechanism by which this IgE suppression occurs is the stimulation and buildup of specific IgG antibodies to the allergen. Scientific research supports the conclusion this IgG “blocking antibody” is the principal reason the patient no longer experiences the allergic reaction.
IgG is called the blocking antibody because the IgE that previously caused the patient’s allergic reaction and symptoms is still there, and but for the IgG getting in the way, would still cause the reaction and symptoms. The levels of specific IgE that was recorded on the patient’s skin test don’t change very much at all, in fact.
Therefore Repeat Skin Testing Is a Mistake: Before After Survey Instead
There is natural tendency to want to confirm the efficacy of allergic immunotherapy by repeating the skin test, expecting the reactions to diminish or disappear. Knowing the mechanism by which immunotherapy works, however, it’s clear that you should not re-skin test the patient. A repeat allergy skin test result on a patient one, two or three years downstream of initiating immunotherapy will not change very much simply because that causal IgE has not decreased even after all that immunotherapy. We see that the patient is clinically better, anyway, which we know because they tell us. Thus, to document the improvement it is highly recommended that your patients fill out the comprehensive Allergy Questionnaire at the beginning of treatment and then have them fill it out on an annual basis, too.
Below is a diagram showing the mechanism how allergen immunotherapy affects the key immune cells. This was shown in my book Dr. Dean Mitchell’s Allergy and Asthma Solution (DeCapo 2006) and reprinted from The Journal of Allergy and Clinical Immunology.
Conclusion: Remember, don’t make the mistake of performing allergy re-skin testing on a patient you are following on allergen immunotherapy–it won’t change, or improve as you might suspect, and the lack of change is unlikely to please your patients even if they feel as though they’re no longer suffering from allergies. Instead, use your Allergy Questionnaires and try to simply explain to the patients they’re clinically better because have successfully developed blocking antibodies.
